Abstract
Introduction: Expression and function of BCL-2 family proteins in multiple myeloma (MM) is important for tumour cell survival and drug resistance, and may partly mediate the protective effect of bone marrow (BM) stroma. Proteasome inhibitors (PIs) are a major class of anti-myeloma drugs, however some patients are resistant and almost all eventually relapse. Carfilzomib is a second generation, irreversible proteasome inhibitor, which is effective in both newly diagnosed and relapsed/refractory disease, but drug resistance and relapse occur.
Aim: We aimed to study the role of BCL-2 family proteins in Carfilzomib (CFZ) mediated cytotoxicity in the presence of stroma, focusing on priming of the pro-apoptotic protein, BIM.
Methods: A panel of Human Myeloma Cell Lines (HMCL) and primary MM cells were exposed to Carfilzomib, and cell death assessed using Annexin V/PI staining and flow cytometry. Co-cultures employing the HS5 stromal cell line were used to model the interaction with stroma. MM cells were exposed to CFZ in a 1hr pulse, to recapitulate the pharmacokinetics of drug exposure in patients. The expression of BCL-2 family proteins was assessed by flow cytometry and Western Blot (WB). The compounds S63845, ABT-199 (Venetoclax) and A-1331852 were used to inhibit MCL-1, BCL-2 and BCL-X L pro-survival proteins respectively. Changes in BIM binding partners were examined by immunoprecipitation and WB.
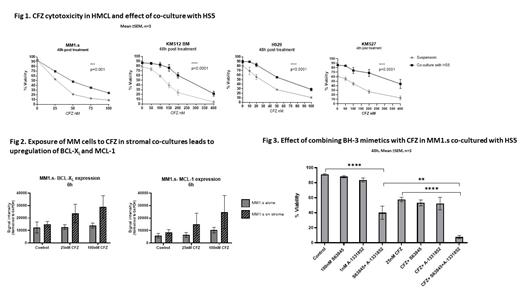
Results: CFZ induced dose and time-dependent cell death of HMCL and primary MM cells. This was primarily mediated by apoptosis as shown by AnV/PI staining (eg. MM1.s at 25nM CFZ: 34±6% apoptosis at 24h, 47±9% at 48h, p=0.016; 50nM CFZ: 60 ±3.8% at 24h vs 79±6% at 48h, p=0.004, mean ±SEM, n=3), and by reduced cytotoxicity in MM1.s BAX/BAK KO cells (100nM CFZ: 10±1% cell death vs 42±5% in WT at 6h, 33±14% vs 99±0.5% at 24h; p=0.0005, n=3). CFZ cytotoxicity was significantly reduced when MM1.s cells were co-cultured with HS-5 (50nM CFZ: 53±4% apoptosis vs 79±4% in suspension, at 48h, p=0.02, n=3) confirming the protective effect of stromal cells. Similar results were seen with H929, KMS27 and KMS12BM HMCL (Figure 1). Co-culture of MM1.s with HS-5 cells induced upregulation of MCL-1 and BCL-X L and downregulation of BCL-2. Combined inhibition of BCL-X L and MCL-1 at concentrations where single agents had minimal effect, resulted in
a marked increase in apoptosis on stroma (Ctrl: 9±1%, S63845 100nM:12±1.4%, A-1331852 1nM: 17±3%, S63845+A-1331852: 60±9%; 48h, p=0.0001, n=3) (Figure 3). BIM immunoprecipitation showed that in the presence of the MCL-1 inhibitor, S63845, there was increased BCL-X L binding to BIM; conversely when BCL-X L was inhibited by A-1331852, an increase in MCL-1/BIM complexes was seen. Exposure of MM cells to CFZ in stromal co-cultures led to a further increase in the expression of BCL-X L and MCL-1. Because BCL-X L and MCL-1 were upregulated both by stromal interaction and by CFZ (Figure 2), we tested the cooperativity of these anti-apoptotic proteins on resistance to CFZ. CFZ-induced cytotoxicity was significantly enhanced by the addition of single BH3 mimetics in the presence of HS-5: cell death 48h, BCL-X L A-133182 5nM: 40±12%, CFZ 25nM: 57±10%, CFZ+A-1331852: 94±2%, p=0.0065, n=3. Cell death with MCL-1 inhibitor S63845 200nM: 12±3%, CFZ 25nM:40±13%, S63845+CFZ: 54±18%, p=0.02, n=3). However, combined BCL-X L and MCL-1 inhibition, using lower concentrations of BH3 mimetics, potently sensitized MM cells to CFZ-mediated cytotoxicity in the presence of stroma (% killing at CFZ 25nM + A-1331852 1nM: 48±8%; CFZ+S63845 100nM: 38±5%; CFZ+A-1331852+S63845: 92±2%, p<0.0001, n=3, Figure 3).
Conclusion: BCL-X L and MCL-1 are upregulated in MM cells by stromal interaction, and also in response to CFZ. The upregulation of pro-survival proteins by stroma may mediate MM cell resistance to PIs, and blockade of both BCL-X L and MCL-1 is required in order to abrogate the protective effect of stroma and restore sensitivity to CFZ. Combination of BH-3 mimetic drugs at subtherapeutic doses with proteasome inhibitors may be a potential therapeutic strategy.
Huang: The Walter and Eliza Hall Institute of Medical Research: Patents & Royalties: Employee of the Walter and Eliza Hall Institute and eligilble for payments in relation to venetoclax. Khwaja: Abbvie: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Astellas: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Jazz Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Pfizer: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Yong: Janssen: Honoraria, Research Funding; Sanofi: Honoraria, Research Funding; Takeda: Honoraria; GSK: Honoraria; Amgen: Honoraria; BMS: Research Funding; Autolus: Research Funding.